The coronavirus pandemic has changed life as we know it in just a few short months. Since the World Health Organisation declared it a Public Health Emergency of International Concern on 30 January, the search for a vaccine has involved thousands of researchers and volunteers around the world. One of the leading candidates is being developed in the UK by a group of Oxford University scientists.
According to the Iran Science Watch (ISW) The Oxford COVID-19 vaccine team is led by Prof Sarah Gilbert, Prof Andrew Pollard, Prof Teresa Lambe, Dr Sandy Douglas, Prof Catherine Green and Prof Adrian Hill. Their team includes scientists from both the Jenner Institute and the Oxford Vaccine Group, who bring together decades of internationally recognised experience in vaccine research, including responding to the Ebola outbreak of 2014.
The teams had already used ChAdOx1 vaccine technology to produce candidate vaccines against a number of pathogens including flu, Zika and Middle East Respiratory Syndrome (MERS), another coronavirus. They had already begun work on pandemic preparedness with the technology behind ChAdOx, in preparation for ‘Disease X’. When the disease emerged in China, they moved quickly. As soon as the genetic sequence was available, they began work on a trial.
How the Oxford COVID-19 vaccine works
The ChAdOx1 vaccine is a chimpanzee adenovirus vaccine vector. This is a harmless, weakened adenovirus that usually causes the common cold in chimpanzees. ChAdOx1 was chosen as the most suitable vaccine technology for a SARS-CoV-2 vaccine as it has been shown to generate a strong immune response from one dose in other vaccines. It has been genetically changed so that it is impossible for it to grow in humans. This also makes it safer to give to children, the elderly and anyone with a pre-existing condition such as diabetes. Chimpanzee adenoviral vectors are a very well-studied vaccine type, having been used safely in thousands of subjects.
Coronaviruses have club-shaped spikes on their outer coats, which form a corona – Latin for crown – on the virus surface. Immune responses from other coronavirus studies suggest that these spikes are a good target for a vaccine.
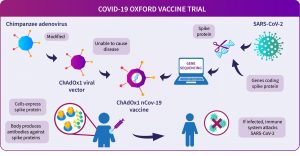
The Oxford vaccine contains the genetic sequence of this surface spike protein. When the vaccine enters cells inside the body, it uses this genetic code to produce the surface spike protein of the coronavirus. This induces an immune response, priming the immune system to attack the coronavirus if it later infects the body.
The Oxford COVID-19 vaccine trials
The main focus of the Phase I, II and III studies is to assess whether the ChAdOx1 vaccine is going to work against COVID-19, that it doesn’t cause unacceptable side effects and if it induces good immune responses.
Adult participants will be randomised to receive one or two doses of either the ChAdOx1 nCoV-19 vaccine or a licensed vaccine (MenACWY) that will be used as a ‘control’ for compariso.
COVID-19 vaccine trial information pages.
To assess whether the vaccine works to protect from COVID-19, the statisticians in our team will compare the number of infections in the control group with the number of infections in the vaccinated group. How quickly we reach the numbers required will depend on the levels of virus transmission in the community. If transmission remains high, we may get enough data in a couple of months to see if the vaccine works, but if transmission levels drop, this could take longer. Recruitment of those who have a higher chance of being exposed to the virus is being prioritised, such as frontline healthcare workers, frontline support staff and public-facing key workers, in an effort to capture the efficacy data as quickly as possible.
Source: University of Oxford
Your email address will not be published. Required fields are marked *